Parasitic infections hit the health of low-income Black communities where states have neglected sewage systems.
Intestinal infections take a heavy toll on impoverished Black communities that have out-of-date sewage systems. These infections often spread through contaminated soil and water and are among the most common diseases worldwide.
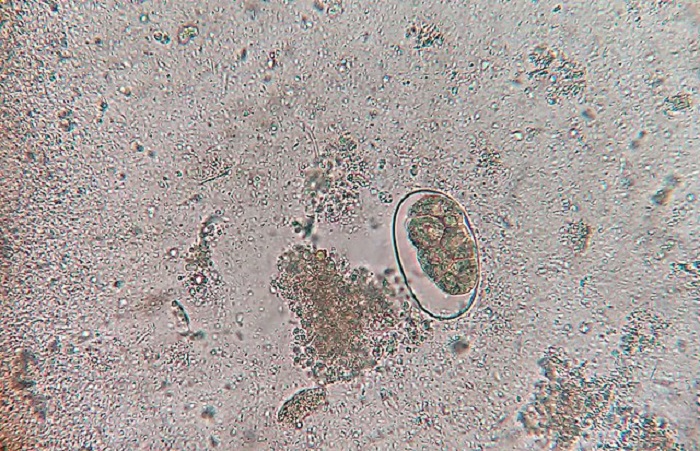
Approximately one-quarter of the global population is infected with soil-transmitted helminths, intestinal parasitic worms that can cause serious health problems.
Additionally, up to 50% of people around the world are infected with Helicobacter pylori, bacteria that live in the stomach and can cause ulcers and cancer.
I am a biological anthropologist, and it is clear to me that these two types of infections contribute to systemic health inequities, especially among communities of color in which limited access to medical care and inadequate sanitation systems may both increase exposure to pathogens and lead to worse outcomes.
Historically, intestinal infections have been prevalent in parts of the U.S. where high poverty rates and environmental factors – such as flooding and warm, humid summers – favor infection spread.
Although many Americans believe these diseases now exist only in lower-income countries, research that my colleague and I have conducted challenges this assumption.
Renewed interest in US intestinal infections
Launched in 2019, the Rural Embodiment and Community Health Study started with the goal of measuring current infection rates and determining which living conditions contribute to infection risk.
Though national infection rates remain unclear because of the absence of large-scale studies, our preliminary work in 2019 found that 38% of children sampled in a predominantly Black Mississippi Delta community had intestinal parasitic infections.
Moreover, 80% of those children exhibited high levels of intestinal inflammation. Those levels are much higher than those observed in other populations and may lead to several poor health outcomes, including impaired intestinal ability to absorb nutrients and stunted growth.
Our more recent analyses from 2022 focused on adults living in the Mississippi Delta and Southwestern Illinois, two areas that experience regular flooding.
Among those adults, 73% displayed elevated intestinal inflammation, while 45% were infected with H. pylori, the bacteria that can cause ulcers and cancer.
Taken together, those results demonstrate widespread intestinal infections and inflammation at all ages in these low-income, mostly Black communities.
Long-lasting intestinal infections and associated inflammation can lead to nutritional deficiencies, restricted growth, reduced educational attainment, decreased work productivity and increased risk for serious diseases later in life, including certain cancers).
A legal challenge in Alabama
The Rural Embodiment and Community Health Study is not alone in recognizing the impact of intestinal infections on Black communities. One of the most widely publicized recent research studies investigating intestinal infections focused on the health effects of poverty and crumbling sanitation infrastructure in Lowndes County, Alabama, a region characterized by a history of racial segregation and inequity.
Researchers found that more than 1 in 3 people tested in Lowndes County were infected with hookworm, an intestinal worm spread through sewage exposure that lives in soil and infects people by burrowing into bare feet.
This 2017 study has since led to legal action.
In a landmark May 2023 court ruling, the Biden administration found that Alabama’s public health department had discriminated against Black residents by denying access to adequate sanitation systems and imposed fines for resulting sewage issues.
This decision is being hailed by environmental justice advocates as a transformative environmental justice agreement that may increase public awareness of the ongoing health crisis that results from infrastructure neglect and associated pathogen exposure.
Community activists – such as Catherine Coleman Flowers, founder of the Center for Rural Enterprise and Environmental Justice – said they hope the federal government continues to intervene, leading to similar results in other affected communities.
“This country’s neglect of wastewater infrastructure in majority Black communities, both urban and rural, is resulting in a hygienic hell for far too many people, a hell that climate change is only making worse,” Flowers said in a March 2023 interview.
Why are there still parasites in the US?
The story of parasite infection in the U.S. is two-sided.
On one hand, the U.S. has successfully controlled many parasite infections. Malaria is one of them.
In addition, advancements in sanitation infrastructure and household construction mean that many Americans do not generally have to worry about parasite infections.
But this national success is not complete, as demonstrated by the recent findings in low-income Black communities across the country.
Limited awareness of the continued threat posed by neglected intestinal infections has made it more difficult to identify and treat these diseases in the U.S. than in lower-income nations.
For instance, in many countries the drugs needed to treat hookworm infections cost mere cents, but in the U.S., where drug prices are unregulated by the federal government, these same medications can cost hundreds of dollars.
The recent court decision in Alabama represents an important step toward increased national recognition of the role intestinal infections play in perpetuating racial health inequities.
Increased awareness will ideally result in improved access to testing and treatment in affected communities. But more work is needed to assess the full extent of these infections across the U.S.
Even if medical treatment is accessible and affordable, vulnerable individuals are often reinfected, as these pathogens continue to spread through the environment. Structural changes are needed to break the cycle of infection and poor health.
Current federal investment in community infrastructure – including water quality – is encouraging but does not go far enough. Ultimately, a concentrated nationwide effort to update and maintain sanitation systems is the best way to finally halt infection transmission and support health equity across the U.S.![]()
Theresa E. Gildner, Arts & Sciences at Washington University in St. Louis
Theresa E. Gildner, Assistant Professor of Biological Anthropology, Arts & Sciences at Washington University in St. Louis
This article is republished from The Conversation under a Creative Commons license. Read the original article.

