
The first three coronavirus vaccines earned Emergency Use Authorization more than a year ago. To date, no other vaccines have been put into use in the U.S – but that will soon change. More than 40 vaccines are undergoing clinical trials in the U.S., employing a number of different approaches to protecting people from the coronavirus. Vaibhav Upadhyay and Krishna Mallela have been studying the coronavirus spike protein since the outbreak of the pandemic and are developing COVID-19 therapeutics. Together, they explain what vaccines are in development and why some of the vaccines should be better than what’s available now.
1. Why are companies working on new vaccines?
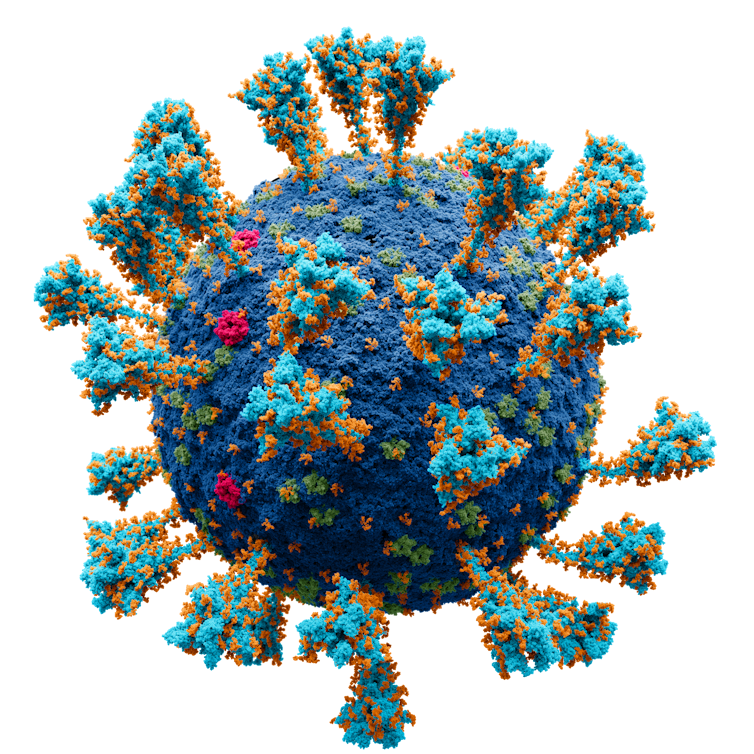
A major reason why new vaccines are important – and why the world is still dealing with COVID-19 – is the continued emergence of new variants. Most of the differences between variants are changes in the spike protein, which is on the surface of the virus and helps it enter and infect cells.
Some of these small changes in the spike protein have allowed the coronavirus to infect human cells more efficiently. These changes have also made it so that previous vaccinations or infections with COVID-19 provide less protection against the new variants. Updated or new vaccines could be better at detecting these different spike proteins and better at protecting against new variants.
2. What kinds of vaccines are in the works?
So far, 38 vaccines have been approved around the world, and the U.S. has approved three of those. There are currently 195 vaccine candidates at different stages of development worldwide, out of which 41 are in clinical trials in U.S. Vaccines against SARS-CoV-2 can be broadly divided into four classes: whole virus, viral vector, protein-based and nucleic acid-based vaccines.
Whole virus vaccines generate immunity using a complete, though weakened – called inactivated or attenuated – SARS-CoV-2 virus. Currently there are two of these vaccines in clinical trials in the U.S. Viral vector vaccines are a variation on this approach. Instead of using the whole coronavirus, they use a modified version of a harmless adenovirus that carries parts of the coronavirus spike protein. The Johnson & Johnson vaccine is a viral vector vaccine, and there are 15 more candidates in this category in clinical trials in the U.S..
Protein-based vaccines use just the spike protein or part of the spike protein to generate immunity. Since the spike protein is one of the most functionally important parts of the coronavirus, an immune response that just targets this one part is sufficient to prevent or overcome an infection. The U.S. currently has five protein-based vaccines undergoing clinical trials.
Nucleic acid-based vaccines are currently the most widely used in the U.S. These are made of genetic material, like DNA or RNA, that codes for the coronavirus’ spike protein. Once a person gets one of these shots, their body reads the genetic material and produces the spike protein. This in turn generates an immune response. There are 17 RNA and two DNA vaccines in clinical trials in the U.S. Some of these are using the genetic material from newer variants, including updated versions of the Moderna and Pfizer vaccines.

3. Will new vaccines be better than existing ones?
The Moderna, Pfizer and J&J vaccines are based on the original strain of the coronavirus and are less potent when facing new variants. Vaccines based on new variants would provide better protection against those newer strains than existing vaccines, and some are under development. Nucleic acid-based vaccines are the easiest to update and make up the majority of variant-targeted vaccines. Moderna has already produced a vaccine that contains mRNA from both the beta and omicron variants, and some recently published clinical data shows that it is more effective against newer variants than Moderna’s original shot.
While updating nucleic acid vaccines is important, some research suggests that viral vector or whole virus vaccines could be more effective against new variants – without the need for updating.
Alexey Solodovnikov, Valeria Arkhipova via WikimediaCommons, CC BY-SA
4. What are the advantages of whole virus vaccines?
Nucleic acid-based and protein-based vaccines use only the spike protein to produce an immune response. With a whole virus vaccine, the immune system not only recognizes the spike protein, but all other parts of the coronavirus, too. The other parts of the virus help to quickly generate a strong immune response that involves many different branches of the immune system and lasts a long time.
Another benefit of whole virus and viral vector vaccines is the ease of storage and shipping. Viral vector vaccines can be stored in common household refrigerators for months, sometimes years. By comparison, the Moderna and Pfizer mRNA vaccines must be stored and shipped at ultra-low temperatures. These infrastructure requirements make whole-virus vaccines much more feasible for use in remote locations of the U.S., as well as across the world.
5. What are some disadvantages of whole virus vaccines?
There are some downsides to whole virus vaccines.
To produce inactivated virus vaccines, you must first produce a huge amount of live coronavirus and then inactivate it. There is a small, but legitimate biohazard risk associated with producing a lot of live coronavirus. A second disadvantage is that inactivated virus and viral vector vaccines might not produce strong protection in immunocompromised patients.
Finally, producing whole virus vaccines is much more labor intensive compared to making mRNA vaccines. You must grow, then purify and then inactivate the virus while carefully checking the quality at each step. This long production process makes it hard to produce large amounts of the vaccine. For the same reasons, redesigning or updating whole-virus vaccines for future variants is more difficult compared to simply changing the code of nucleic acid-based or protein-based vaccine.
Looking at the pros and cons of each vaccine type, we believe virus-based vaccines could play an important role in generating a long-lasting, broad immunity against a rapidly mutating virus. But easily updated mRNA or protein-based approaches that can be fine-tuned to the latest variants can also be key in containing the spread of the pandemic. With vaccines of all types in the works, public health officials and governments around the world will have more tools at their disposal to deal with whatever the coronavirus brings next.
Vaibhav Upadhyay, University of Colorado Anschutz Medical Campus and Krishna Mallela, University of Colorado Anschutz Medical Campus
Vaibhav Upadhyay, Postdoctoral Fellow of Pharmaceutical Science, University of Colorado Anschutz Medical Campus and Krishna Mallela, Professor of Pharmaceutical Science, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.