Even before the pandemic, there was plenty for expectant mothers to worry about. Pregnant women must withstand a barrage of arguably well-intentioned, but often hyperbolic, warnings about their health and what’s to come, including concerns about everything from what to eat, to what to wear, to how to feel. Health professionals know that mothers-to-be experience predictable increases in anxiety levels before infants are born. Maternal mental health has been steadily deteriorating in the U.S., particularly among poor and minority women.
The calls to “be afraid, be very afraid” are, of course, countered by the equally strong cautions for pregnant women to not worry too much, lest it lead to long-term negative outcomes for them and their infants.
Such warnings are not entirely off base. Maternal stress hormones cross the placenta and affect the vulnerable fetus. Fetal exposure to the stress hormone cortisol has been linked to an array of negative outcomes, including miscarriage and preterm birth, and irritable temperament for the child and increased risk of emotional problems during childhood. One thing researchers know is that anxious mothers tend to have anxious children. This common, albeit not prescriptive, phenomenon is likely due to numerous factors, both pre- and postpartum.
In our laboratory, we focus on what happens when women start their pregnancies already worried or anxious and what clues we can uncover about how to help them and their children. Our research suggests that worry during pregnancy can have long-term impacts on how mothers’ brains communicate – but also that there might be some simple steps that can help rein in the effects.
Maternal brains change during pregnancy
The fetal brain isn’t the only one that is vulnerable during pregnancy. There’s evidence that the maternal brain reorganizes in ways that likely prepare a pregnant woman to care for another human being. The experience of stress during pregnancy can thus hijack a period of change meant to allow for positive adaptations and instead open the door for anxiety problems.
We are interested in whether there might be easy, approachable ways to offset some of these negative effects. So we invite pregnant women into our lab, where we can record their naturally occurring brain activity using electroencephalography. This EEG technique gives us a great sense of how quickly and how strongly brains react to particular stimuli.
In a recent study from our lab, we measured pregnant women’s neural reactivity while they viewed emotional and nonemotional pictures. For most people, including pregnant women, their brains show more activity when they’re presented with a negative image or sound – like a crying baby – than with a neutral image or sound – such as a blanket.
We found that for some women in their third trimester of pregnancy, this effect was disrupted; instead of reacting more strongly to a negative image, expectant mothers’ brains showed the same response to negative and neutral pictures. Basically these mothers-to-be did not, at the neural level, distinguish neutral from negative images.
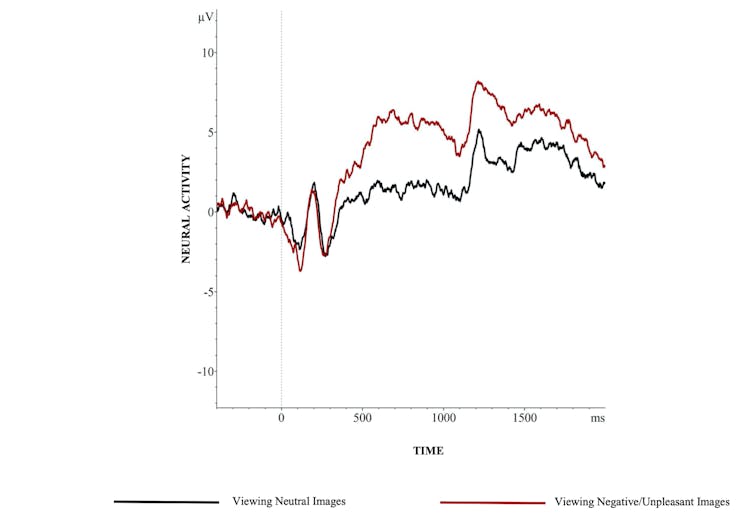
We can’t be sure whether what we observed was these women’s brains reacting to neutral pictures as though they were negative, or to negative pictures as though they were neutral. But we did see that the difference between the two emotional categories was smaller compared to what we would expect.
In the context of our interest in worry and anxiety, this finding is concerning. It looks like these women are at risk of responding to even nonthreatening information as though it is problematic. That is, the line between what is worrisome and what should not be becomes blurred, even at the level of neural activity. Other research suggests that this may hurt the mother-infant relationship over time. Researchers found that when women’s brains were more reactive to neutral information, similar to what we think may be happening in our study, mothers reported more difficulty interpreting emotions in their infant.
Critically, though, we saw this mixed-up reaction only in pregnant women who reported having low levels of social support. We asked our volunteers to create lists of people they felt they could talk to if they were in a difficult situation or needed help. We also asked them to tell us if they thought, as they reflected on these lists, that the social support available to them was adequate. When women reported more satisfaction with their social support networks, the neural response was just as we expected, with a clear distinction between negative and neutral information.
Our findings are consistent with studies of nonpregnant individuals, suggesting that adequate social support calms the body’s responses to stress. Our work identifies social support as a specific and easily targeted step for protecting pregnant women in ways that can influence neural function during a sensitive period of reorganization.
Adequate support is in the eye of the beholder
What especially caught our eye in these findings is that we used a measure of social support that was based on a woman’s perception about how much backup was available to her should she need it. Whether or not her belief is accurate is unknown.
However, more and more neuroscientific evidence underscores the degree to which people live in their own subjective realities. It is intuitive, and supported by decades of work in sociology and social psychology, that people base their thoughts, feelings and actions on what they believe to be true about the world regardless of whether it’s accurate.
In this case, a woman’s feelings about her available social support are based on how good she feels about that network rather than whether anyone else thinks she has enough people to talk to if a problem arises.
It follows, then, that changing a mom-to-be’s perception that she has sufficient social support can change the way that her brain processes emotional information to make it more closely resemble typical, healthy function.
Our research suggests there’s an easy and inexpensive way to support pregnant mothers that can alter neural reactivity to negative information and may serve to protect both maternal and child outcomes – simply help mom feel more supported. That doesn’t need to mean encouraging women to join clubs or groups or find new friends or therapists. Rather, pregnant women may benefit from simply recognizing the power and benefit of the networks they already have in place.
Rebecca Brooker, Texas A&M University and Tristin Nyman, Texas A&M University
Rebecca Brooker, Associate Professor of Psychological and Brain Sciences, Texas A&M University and Tristin Nyman, Ph.D. Student in Psychological & Brain Sciences, Texas A&M University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
