
After months battling the COVID-19 pandemic, the idea of “herd immunity” is back in the news.
This has been stoked by reports about the White House’s new pandemic advisor, Scott Altas, who has argued in favor of ending social isolation measures and simply allowing healthy people to get infected. The idea is that the virus wouldn’t spread as quickly once enough people became immune. But trying to reach herd immunity without a vaccine would be a disastrous pandemic response strategy.
As mathematics and computer science professors, we think it is important to understand what herd immunity actually is, when it’s a viable strategy and why, without a vaccine, it cannot reduce deaths and illnesses from the current pandemic.
What is herd immunity?
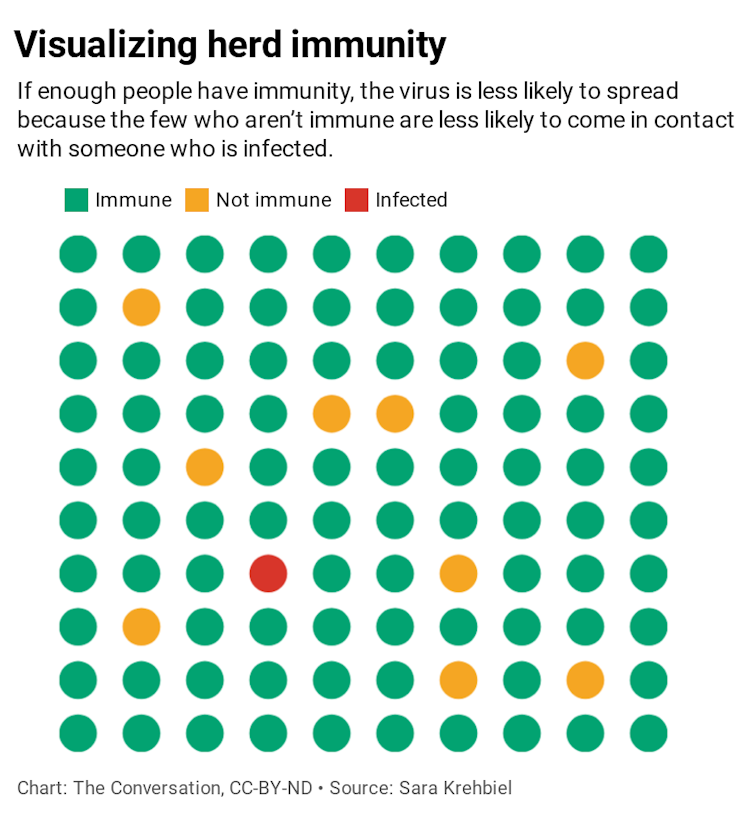
Epidemiologists define the herd immunity threshold for a given virus as the percentage of the population that must be immune to ensure that its introduction will not cause an outbreak. If enough people are immune, an infected person will likely come into contact only with people who are already immune rather than spreading the virus to someone who is susceptible.
Herd immunity is usually discussed in the context of vaccination. For example, if 90% of the population (the herd) has received a chickenpox vaccine, the remaining 10% (often including people who cannot become vaccinated, like babies and the immunocompromised) will be protected from the introduction of a single person with chickenpox.
But herd immunity from SARS-CoV-2 is different in several ways:
1) We do not have a vaccine. As biologist Carl Bergstrom and biostatistician Natalie Dean pointed out in a New York Times op-ed in May, without a widely available vaccine, most of the population – 60%-85% by some estimates – must become infected to reach herd immunity, and the virus’s high mortality rate means millions would die.
2) The virus is not currently contained. If herd immunity is reached during an ongoing pandemic, the high number of infected people will continue to spread the virus and ultimately many more people than the herd immunity threshold will become infected – likely over 90% of the population.
3) The people most vulnerable are not evenly spread across the population. Groups that have not been mixing with the “herd” will remain vulnerable even after the herd immunity threshold is reached. Furthermore, it is impossible to fully isolate vulnerable populations while everyone else goes back to normal.
Reaching herd immunity without a vaccine is costly
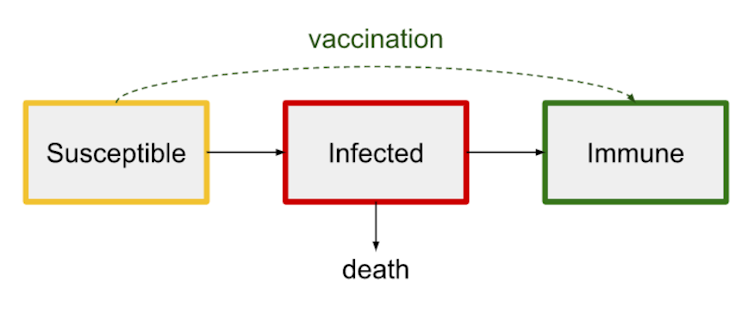
For a given virus, any person is either susceptible to being infected, currently infected or immune from being infected. If a vaccine is available, a susceptible person can become immune without ever becoming infected.
Without a vaccine, the only route to immunity is through infection. And unlike with chickenpox, many people infected with SARS-CoV-2 die from it.
By Sept. 1, more than 184,000 people in the U.S. had died from COVID-19. This figure includes children and others in low-risk groups, and the disease can have lingering health consequences for those who survive. Moreover, scientists don’t yet know the extent to which people who recover are immune from future infections.
A vaccine is the only way to move directly from susceptibility to immunity, bypassing the pain from becoming infected and possibly dying.
Herd immunity reached during a pandemic doesn’t stop the spread
An ongoing pandemic doesn’t stop as soon as the herd immunity threshold is reached. In contrast to the scenario of a single person with chickenpox entering a largely immune population, many people are infected at any given time during an ongoing pandemic.
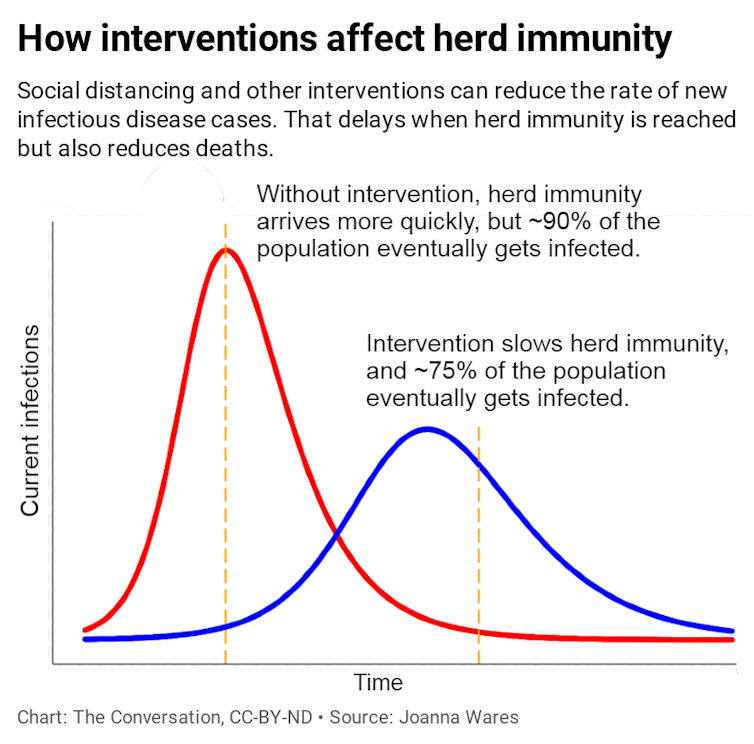
When the herd immunity threshold is reached during a pandemic, the number of new infections per day will decline, but the substantial infectious population at that point will continue to spread the virus. As Bergstrom and Dean noted, “A runaway train doesn’t stop the instant the track begins to slope uphill, and a rapidly spreading virus doesn’t stop right when herd immunity is attained.”
If the virus is unchecked, the final percentage of people infected will far overshoot the herd immunity threshold, affecting as many as 90% of the population in the case of SARS-CoV-2.
Proactive mitigation strategies like social distancing and wearing masks flatten the curve by reducing the rate that active infections generate new cases. This delays the point at which herd immunity is reached and also reduces casualties, which should be the goal of any response strategy.
Herd immunity does not protect the vulnerable
People who are particularly vulnerable to COVID-19, such as people over 65, have been urged to stay inside to avoid exposure. But full isolation in our society is impossible, so the greater the number of active cases, the greater the risk to these vulnerable people.
Even if the herd immunity threshold is reached by the population at large, a single infected person coming in contact with a vulnerable community can cause an outbreak. The coronavirus has devastated nursing homes, which will remain vulnerable until vaccines are available.
How to respond to a pandemic without a vaccine
Without a vaccine, we should not think of herd immunity as a light at the end of the tunnel. Getting there would result in many more needless deaths in the United States and would not protect the most vulnerable.
For now, testing and contact tracing, wearing masks, and social distancing remain the best ways to lessen the destruction of COVID-19 by flattening the curve to buy time to develop treatments and vaccines.
This article has been updated with details about the White House’s new pandemic advisor.
Joanna Wares, University of Richmond and Sara Krehbiel, Santa Clara University
Joanna Wares, Associate Professor of Mathematics, University of Richmond and Sara Krehbiel, Assistant Professor of Mathematics and Computer Science, Santa Clara University
This article is republished from The Conversation under a Creative Commons license. Read the original article. https://creativecommons.org/licenses/by-nd/4.0/